Scientists with City of Hope®, one of the largest cancer research and treatment organizations in the United States, and the Translational Genomics Research Institute (TGen), part of City of Hope, may have discovered one of the causes for a type of leukemia to develop into a more aggressive form, according to recent research published in Nature Communications.
Led by Guido Marcucci, M.D., City of Hope professor and chair, Department of Hematologic Malignancies Translational Science, director, Gehr Family Center for Leukemia Research, and chief, Division of Leukemia, and Bin Zhang, Ph.D., associate professor, City of Hope’s Department of Hematologic Malignancies Translational Science, the research team analyzed the RNA of chronic myeloid leukemia cells (CML) and found that miR-142, an RNA molecule that regulates cell metabolism, was missing.
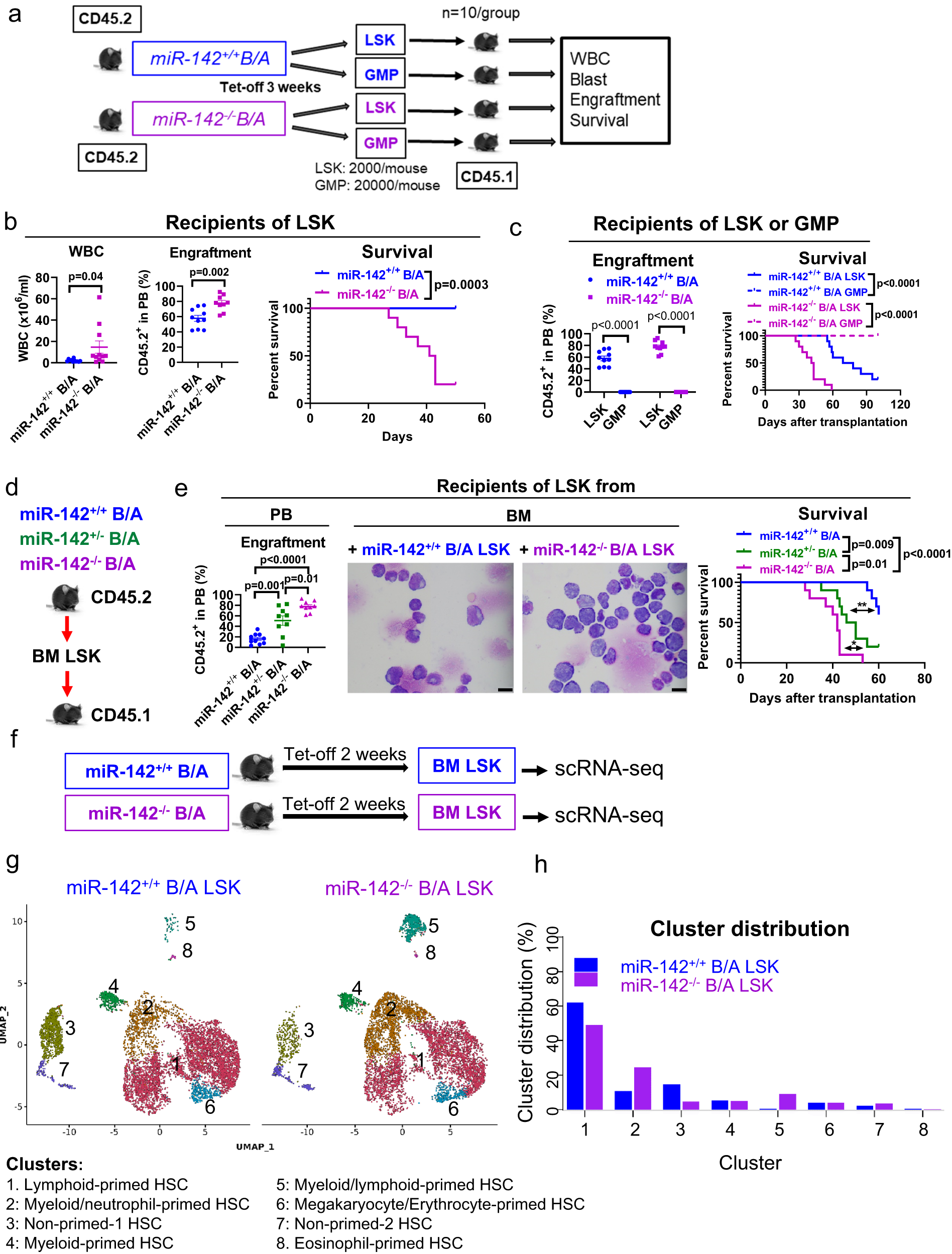
Identification and single cell gene expression profiles of BC-LSCs vs CP-LSCs
a–c Schematic design and results of the experiment. a LSK (2000/mouse, n = 10 mice per group) and GMP (20,000/mouse, n = 10 mice per group) populations from CD45.2 miR-142−/−BCR-ABL and miR-142+/+BCR-ABL mice (BCR-ABL were induced for 3 weeks) were transplanted into congenic CD45.1 wt recipients. b White blood cell (WBC) counts (p = 0.04), peripheral blood (PB) engraftment rates (CD45.2+, p = 0.002) by flow cytometry measured at four weeks after transplantation, and survival (Log-rank test, p = 0.001) of recipients transplanted with LSKs from miR-142−/−BCR-ABL or miR-142+/+BCR-ABL mice (n = 10 mice per strain) are shown. c PB engraftment rates (CD45.2+, p < 0.0001) at four weeks post transplantation and survival (Log-rank test, p < 0.0001) of recipients transplanted with LSKs or GMPs from miR-142+/+BCR-ABL and miR-142−/−BCR-ABL mice (n = 10 per group) are shown. d, e Schematic design and results of the experiment. d LSKs from CD45.2 miR-142−/−BCR-ABL, miR-142+/−BCR-ABL and miR-142+/+BCR-ABL mice (BCR-ABL were induced for 3 weeks) were transplanted into congenic CD45.1 wt recipients. e PB engraftment rates at 4 weeks post transplantation, BM blasts assessed by microscopy (scale bar: 10 µM), and survival of these recipient mice are shown (n = 10 mice per group; Log-rank test, miR-142−/−B/A vs miR-142+/−B/A: p = 0.01; miR-142+/−B/A vs miR-142+/+B/A: p = 0.009; miR-142−/−B/A vs miR-142+/+B/A: p < 0.0001). For b, c, e, h, source data are provided as a Source Data file. For e, results from one of the three independent experiments are shown (n = 3). For b, c, e, comparison between groups was performed by two-tailed, unpaired t-test. Results shown represent mean ± SEM. Significance values: *p < 0.05; **p < 0.01. f–h Schematic design and results of the experiment. f BM LSK cells from miR-142−/−BCR-ABL and miR-142+/+BCR-ABL mice (BCR-ABL were induced for two weeks) were sorted for scRNA-seq. g LSK clusters and h cluster cell distribution are shown. B/A BCR-ABL, tet-off tetracycline withdrawal, GMP granulocyte-macrophage progenitors, PB peripheral blood, BM bone marrow, scRNA-seq single cell RNA sequencing, SEM standard error of the mean.
Researchers hypothesized that the exclusion of this small RNA molecule has important implications as it allows CML cells to expand and eventually develop into a more aggressive form of the disease called blastic phase (BP), which is the equivalent of secondary acute myeloid leukemia (sAML), and is deadly with limited treatment options.
The team developed a synthetic version of miR-142 and tested it in mouse models of BP CML. They found that adding miR-142 prevented CML transformation and some mice with BP CML were even cured of their disease.
Researchers also found that adding tyrosine kinase inhibitors, which is a Food and Drug Administration-approved therapy for CML, increased the anti-leukemic activity of the synthetic miR-142.
“What’s exciting is that we have potentially discovered how we can knock down the leukemia stem cells, which are the equivalent ‘queen bees’ of the disease, and how we can keep them from producing more cancer cells,” Zhang said.
The only current curative option for CML that has developed into BP is a blood marrow or stem cell transplant. A transplant may not work in some patients or can create serious side effects.
“More options are urgently needed for these patients. Our team will now work on developing synthetic miR-142 therapy for use in patients in clinical trials, hopefully as soon as next year,” Marcucci said.
Leveraging TGen’s unique molecular profiling platforms, this study also uncovered that the loss of mIR-142 in CML causes major changes in the tumor metabolism.
“These key metabolic changes are at the heart of the transformation of CML into blast crisis, which, unfortunately, is associated with poor treatment options,” said Patrick Pirrotte, Ph.D., associate professor at TGen and director of City of Hope’s Integrated Mass Spectrometry Shared Resource. “These new molecular findings provide interesting new avenues for therapies.”
The CML research can be applied to finding better treatments for myeloproliferative neoplasms since both are diseases of the bone marrow.
Source – City of Hope
Zhang B, Zhao D, Chen F, Frankhouser D, Wang H, Pathak KV, Dong L, Torres A, Garcia-Mansfield K, Zhang Y, Hoang DH, Chen MH, Tao S, Cho H, Liang Y, Perrotti D, Branciamore S, Rockne R, Wu X, Ghoda L, Li L, Jin J, Chen J, Yu J, Caligiuri MA, Kuo YH, Boldin M, Su R, Swiderski P, Kortylewski M, Pirrotte P, Nguyen LXT, Marcucci G. (2023) Acquired miR-142 deficit in leukemic stem cells suffices to drive chronic myeloid leukemia into blast crisis. Nat Commun 14(1):5325. [article]